Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Full access to educational content, events and resources
- Track your progress
- Share content with your colleagues
- Share supporting material with your patient
What is wound infection?
A wound is considered infected when microorganisms that damage local tissue and delay wound healing are present.1
The presence of microorganisms triggers an immune response in the patient. Whether or not this response is successful depends on a balance of two things:
- the strength of the patient’s immune system; and
- the amount and virulence of the pathogens.
What causes wound infection?
When the amount and virulence of the pathogens are too much for the patient’s immune system to handle, the wound becomes infected.2
What role do microorganisms play in a wound?
It’s important to note that all wounds contain microorganisms, and their presence does not necessarily mean the wound is infected. Wound infection occurs when microorganisms move deeper into the wound tissue and proliferate leading to local and / or systemic immune response.
Keep in mind that:
- a wound’s bacterial status can change depending on local, environmental and systemic factors; and
- the transition from non-infected to infected wounds is often gradual.
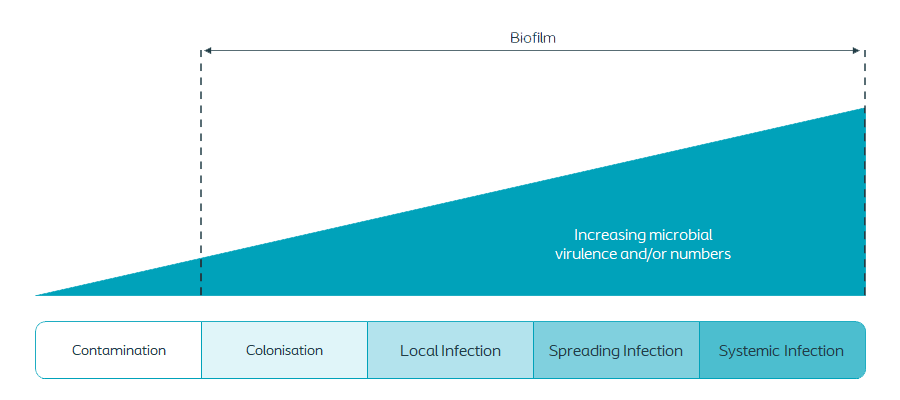
Stages in wound infection
Contamination: The wound is considered contaminated when non-proliferating microorgganisms are present.1
In a contaminated wound:
- The host defence destroys the microorganisms
- There are no specific clinical signs / symptoms of infection6
- There is a steady state of microorganisms5
Colonisation
- The microorganisms in the wound undergo limited proliferation no significant host response 1
- The bacteria grow and multiply at a non-critical level, not damaging tissue and having no significant effect on wound healing 1,5
Local Infection
- The microorganisms proliferate and move deeper into the wound bed and tissue causing a host response1
- The response is localised in one location, system or structure1
- Microorganisms in the wound are multiplying5
- The signs and symptoms are subtle, but may develop into classic symptoms of infection1
| Subtle symptoms1 | Classic symptoms infection1 |
|---|---|
|
|
Spreading Infection
- Microorganisms are present within the wound and are proliferating and invading the surrounding tissues 1
- The patient1 will show subtle as well as classic symptoms and may also demonstrate early systemic infection indicators
Systemic Infection
- Systemic infection from a wound affects the body as a whole, with microorganisms spreading throughout the body via the vascular or lymphatic systems 1
- Signs and symptoms of systemic infection are:1
- Sepsis
- Organ dysfunction
- Systemic inflammatory response
How do you treat an infection?
If you suspect an infection, your immediate goal is to reduce the bioburden in the wound.3 You can do this by:
- therapeutic cleansing of the wound at each dressing change;
- aggressive debriding the surface substance and underlying non-viable or unhealthy tissue. This will disrupt the microbial burden and prevent biofilmfrom reoccurring;3 and
- monitor the wound’s progress and reassess it continually to see if the wound is meeting your treatment goals. You should do this at least once a week or, optimally, at each dressing change.4
What are the clinical signs of wound infection?
In the chart, you’ll see a list of the clinical signs and symptoms of local and systemic infections that you need to look out for when assessing the wound.2:
| Signs of local infection | Signs of systemic infection |
|---|---|
|
|
If a wound still shows these signs of infection after it has been managed correctly and the patient has received appropriate health support, biofilm may be present.
Reducing the risk of wound infection
- Early identification and treatment to reduce or eliminate infection is clinically and economically beneficial to facilitate wound healing and reduce the impact on the patient and on healthcare systems.
- A holistic and collaborative approach is vital to the delivery of best practice.
- Collaborating with the patient in care decisions can help reduce the physical and psychosocial impacts of wound infection.
- Identifying the risk factors through assessment and then addressing them through education with the patient are essential.
A comprehensive wound infection prevention and treatment plan should develop from a holistic assessment and should address:
- Optimising the individual host response
- Reducing local microbial burden
- Promoting a positive environment for wound healing
Who is at risk of a wound infection?
Development of a wound infection is multifactorial and occurs when the cumulative risk factors overwhelm the host defence system.1
Factors that debilitate the patient, impair immune response or reduce tissue perfusion increase the risk of infection.5
| Individual | Environmental |
|---|---|
|
|
To combat the above individual factors, its important to create your optimal host response. You can do this in the following ways.
- Managing comorbidity (diabetes, enhance tissue oxygenation / perfusion)
- Optimise nutritional status & hydration
- Seek and treat other sites of infection
- Provide systemic antimicrobial if necessary
- Manage pain & fever
- Educate patient & carer
- Ensure psychosocial support
- Ensure patient cooperation
- Minimise or eliminate risk factors
To combat the above environmental factors, consider the following measures.
- Provide wound care in a clean environment
- Determine the appropriate aseptic technique based on risk assessment of the patient, wound and environment
- Provide patient and carer education
- Review policies and procedures
- Store equipment appropriately
