Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
- Full access to educational content, events and resources
- Track your progress
- Share content with your colleagues
- Share supporting material with your patient
The two conditions that lead to diabetic foot disease
Let’s take a look at how these two disorders lead to the formation of a diabetic foot ulcer.
Peripheral diabetic neuropathy – losing protective sensation
Peripheral diabetic neuropathy occurs when the sensory, motor and autonomic nerves of the peripheral nervous system don’t function properly in people with diabetes. Peripheral diabetic neuropathy is normally diagnosed when other causes have been excluded. Some patients experience painful sensory neuropathy, which includes a burning or tingling sensation known as paraesthesia.5
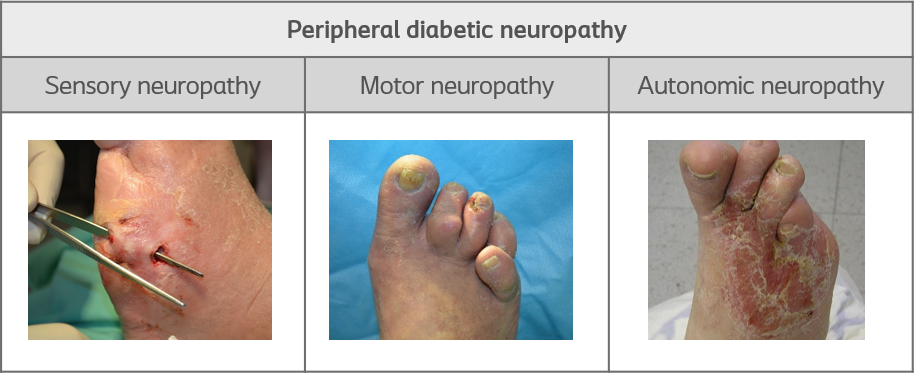
Peripheral diabetic neuropathy explained:
- is a result of poor glucose control
- is a common long-term complication in people with diabetes
- increases the risk of ulceration sevenfold
People with Peripheral diabetic neuropathy can’t feel:5
- temperature changes
- vibrations
- proprioception (i.e. the body’s movement or position)
- pressure
- pain
Peripheral arterial disease - injuries are slow to heal
Peripheral arterial disease is another complication of diabetes. In Peripheral arterial disease, fatty deposits build up in the arteries. These deposits keep blood from flowing to the leg muscles.8 This lack of adequate blood flow prevents leg ulcers from healing.5 So when a chronic leg ulcer develops, this can lead to infection and amputation.
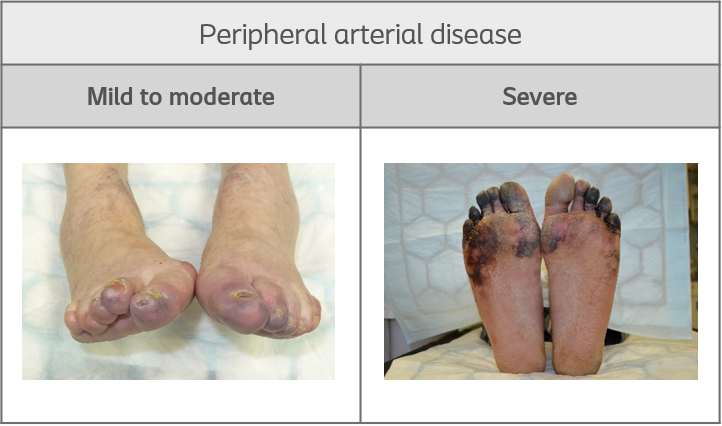
How do I know my patient has Peripheral arterial disease?
If your patient has diabetes, consider the following:
- Do they complain of weakness in the legs?
- Do they experience thigh or muscle pain or cramps (i.e. intermittent claudication) when walking?
If your patient answers ‘yes’ to these questions, he or she might have Peripheral arterial disease. The symptoms can range from asymptomatic to gangrene in the legs. However, most patients that have Peripheral arterial disease are not aware of it, so they don’t seek treatment.5
How Peripheral diabetic neuropathy affects blood flow
This picture illustrates how fatty deposits build up in the arteries. These deposits restrict the blood flow in the legs.
Did you know?
PAD is present in up to 50% of patients with a diabetic foot ulcer.
References
View references
- Price, P. (2004). The Diabetic Foot: Quality of Life. Clinical Infectious Diseases. 39, 129–31.
- Raghav, A., Ahmad Khan, Z., Kumar Labala, R., Ahmad, J., Noor, S., Kumar Mishra, B. (2019). Financial burden of diabetic foot ulcers to world: a progressive topic to discuss always. Ther Adv Endocrinol Metab. 9(1) 29–31.
- Ahmad, A., Abujbaraa, M., Jaddouc, H., Younesd, N. A. (2018). Anxiety and Depression Among Adult Patients With Diabetic Foot: Prevalence and Associated Factors. J Clin Med Res. 10(5):411-418.
- Schaper, N. C., van Netten, J. J., Apelqvist, J., Bus, S. A., Hinchliffe, R. J., Lipsky, B. A. on behalf of the International Working Group on the Diabetic Foot (IWGDF) (2019). IWGDF Practical guidelines on the prevention and management of diabetic foot disease.
- International Diabetes Federation (2017). Clinical Practice Recommendation on the Diabetic Foot: A guide for health care professionals: International Diabetes Federation: Brussels
- National Institute for Health and Care Excellence (NICE) (2015). Diabetic foot problems: Prevention and management.
- Pendsey, S. P. (2010). Understanding diabetic foot. Int J Diabetes Dev Ctries. Apr-Jun; 30(2): 75–79.
- Tawfik, M. (2017). Peripheral arterial disease and the diabetic foot. Diabetic Foot Canada 5: 10–13.
- World Union of Wound Healing Societies (WUWHS) (2016). Florence Congress, Position Document. Local management of diabetic foot ulcers. Wounds International.
- Wounds International (2013). International Best Practice Guidelines: Wound Management in Diabetic Foot Ulcers.
- Dowsett, C., Protz, K., Drouard, M. and Harding, K. G. (2015). Triangle of Wound Assessment made easy. Wounds International, May.
