Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
![]() Full access to educational content, events and resources
Full access to educational content, events and resources
![]() Track your progress
Track your progress
![]() Share content with your colleagues
Share content with your colleagues
![]() Share supporting material with your patient
Share supporting material with your patient

Newsletter
Living with a parastomal bulge
– The patients’ perspective
This article is based on a presentation given by Marianne Krogsgaard, PhD student (Denmark) at the Coloplast Ostomy Days 2018
Marianne has worked as a colorectal nurse for more than 20 years. Her PhD research focuses on colorectal surgery from a patient perspective, with specific reference to parastomal hernia as a late complication after stoma formation. Marianne is currently employed at the Abdominal Centre, Rigshospitalet, Denmark, and since 2015, she has also been the daily manager of the Danish Stoma Database Capital Region.
Very little is known about the impact a parastomal bulge has on a person’s life. In this article, we share the results of a qualitative study that sheds light on life with a parastomal bulge – from the patient’s point of view. We also identify the need for more research into nursing interventions that can reduce symptoms and improve quality of life for this particular group of patients.
Patient profile and incidence rates
The typical profile of someone with a parastomal bulge is a male, over 60 years of age, with a colostomy1-4. There are also a number of other predisposing factors – for example patient factors, (e.g. malnutrition and smoking); disease factors (e.g. diabetes and hypertension); and technical factors related to stoma creation (e.g. laparoscopic surgery and aperture size). However, none of these factors are well-established1, 5-9. It is still unknown which ones matter the most – and whether or not it has any effect if they are modified prior to surgery.
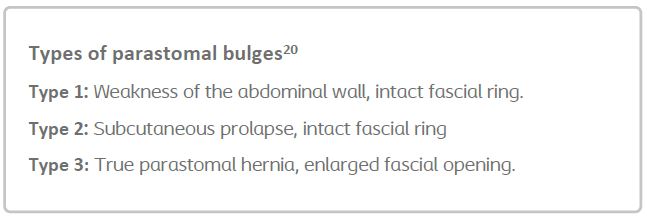
There are several factors that make it difficult to identify the overall incidence rate with any certainty. Incidence rates depend on definitions – that is, if it’s a bulge or a hernia. They also depend on how the incident is reported – whether it is self-reported; identified during a clinical examination; or diagnosed with a CT scan.
What is well known, however, is that the incidence of parastomal bulge increases over time4. A study using data from the Danish Stoma Database Capital Region, with more than 5,000 stoma patients, showed a cumulative incidence of parastomal bulging after just a year of 36 per cent1. The study also found that patients with a colostomy had a 40 per cent higher risk of a parastomal hernia when compared with patients with an ileostomy.

Impact on quality of life
When it comes to symptoms in relation to a parastomal bulge, descriptions vary significantly. Some studies report that patients are mainly asymptomatic, and others state that patients are primarily symptomatic10-15. It all depends on which patients are included and what questions are asked.
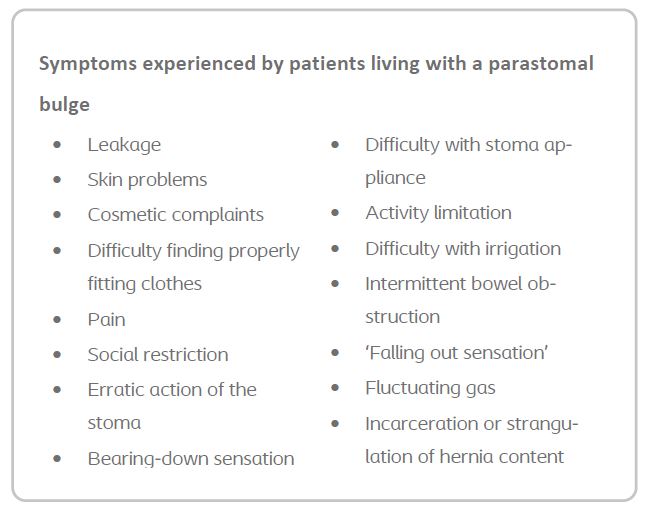
The importance of asking the right questions was revealed by a study conducted at Bispebjerg Hospital, where nurses systematically interviewed patients about their symptoms the day before a parastomal hernia repair16. They found that patients reported a number of different symptoms, and they also detected a high symptom load – i.e. each patient had a number of different symptoms. Three of the symptoms captured in the study – erratic action of the stoma, bearing-down sensation and activity limitation – are not frequently reported in studies. So if a patient has these symptoms, and isn’t asked about them, he may mistakenly be categorised as ‘asymptomatic’.
“Unless we have a very systematic approach, it may not be quite sufficient to only rely on clinician-reported outcomes,” explains Marianne. “If we want to get insight into the patient’s perspective, we need reports coming directly from the patients.”
Getting the patient perspective
To gain more insight into how living with a parastomal bulge impacts patients’ quality of life, Marianne conducted a qualitative study where patients were asked about their symptoms17. The study revealed a wide range of physical and emotional effects of living with a parastomal bulge.
The physical impact
Patients living with a bulge experience unfamiliar and unpleasant bodily sensations. These included altered bowel habits and fluctuating noisy gas that impacted their daily lives. The patients described unpleasant sensations, such as bearing down, where they feel fine in the morning, but heaviness at the end of the day. Some felt like their organs were falling out of their abdomen when they lifted their arms above their head or when they lay on their side. They classified pain into different categories: pain when lifting, pain because of stretching skin and when passing stool.
The psychological impact
Patients felt that the ever-changing bulge required their constant attention. They worried about whether or not it would stop growing. Patients also described the impact the bulge had on their body self-image. Some stated that they felt deformed, deviant and asymmetric. They described the bulge as ‘a woman’s breast’, ‘a melon’ or ‘a cone’. The more the patients perceived that the bulge altered their body image, the harder it was for the patients to adjust to the bulge.
How they coped
Patients took practical measures to deal with their bulge. They would modify their clothing, and they would try to use coping mechanisms like humour and creativity to take charge of their condition. Every time the bulge grew, patients would have to change products, procedures and garments. To deal with this, they needed access to stoma care nurses. Being able to quickly and easily engage with professional staff was a way for patients to regain control over their bulge and remaster the art of self-care.
Need for research into best-practice nursing interventions
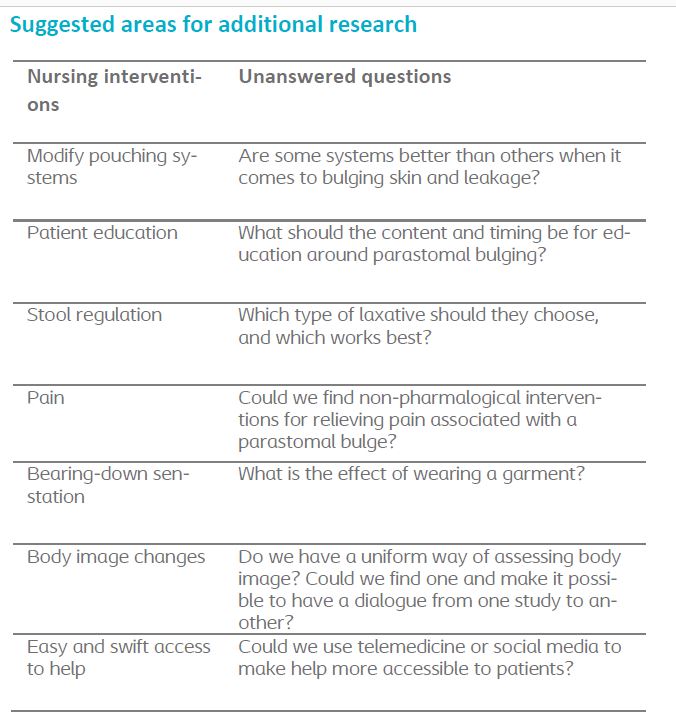
Now that Marianne’s study, along with several others18-19, have shown that a parastomal bulge impacts patients’ lives, the next step is to identify the kinds of nursing interventions that can relieve the situation and help patients manage their parastomal bulging.
This is where we run short on evidence-based know-how. There is an absence in the literature when it comes to documented, best-practice nursing interventions that can improve patients’ quality of life. We find descriptions of interventions, but they are all based on expert opinion and clinical experience.
“If we want an evidence-based nursing culture, we really need research into interventions that can reduce patients’ symptoms, improve their quality of life, and impact their daily lives,” says Marianne. “The focus needs to be on the patient’s perspective. We need to publish and share to get closer to solutions to this problem.”
References
- Andersen RM, Klausen TW, Danielsen AK, Vinther A, Gogenur I, Thomsen T. Incidence and Risk Factors for Parastomal Bulging in Patients with Ileostomy or Colostomy: a Register-based Study using data from the Danish Stoma Database Capital Region. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2017.
- Hong SY, Oh SY, Lee JH, Kim do Y, Suh KW. Risk factors for parastomal hernia: based on radiological definition. Journal of the Korean Surgical Society. 2013;84(1):43-7.
- Mylonakis E, Scarpa M, Barollo M, Yarnoz C, Keighley MR. Life table analysis of hernia following end colostomy construction. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2001;3(5):334-7.
- Londono-Schimmer EE, Leong AP, Phillips RK. Life table analysis of stomal complications following colostomy. Diseases of the colon and rectum. 1994;37(9):916-20.
- Hotouras A, Murphy J, Power N, Williams NS, Chan CL. Radiological incidence of parastomal herniation in cancer patients with permanent colostomy: what is the ideal size of the surgical aperture? International journal of surgery (London, England). 2013;11(5):425-7.
- Pilgrim CH, McIntyre R, Bailey M. Prospective audit of parastomal hernia: prevalence and associated comorbidities. Diseases of the colon and rectum. 2010;53(1):71-6.
- Nastro P, Knowles CH, McGrath A, Heyman B, Porrett TR, Lunniss PJ. Complications of intestinal stomas. The British journal of surgery. 2010;97(12):1885-9.
- De Raet J, Delvaux G, Haentjens P, Van Nieuwenhove Y. Waist circumference is an independent risk factor for the development of parastomal hernia after permanent colostomy. Diseases of the colon and rectum. 2008;51(12):1806-9.
- Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. The British journal of surgery. 2003;90(7):784-93.
- Ripoche J, Basurko C, Fabbro-Perray P, Prudhomme M. Parastomal hernia. A study of the French federation of ostomy patients. Journal of visceral surgery. 2011;148(6):e435-41.
- Moreno-Matias J, Serra-Aracil X, Darnell-Martin A, Bombardo-Junca J, Mora-Lopez L, Alcantara-Moral M, et al. The prevalence of parastomal hernia after formation of an end colostomy. A
- new clinico-radiological classification. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2009;11(2):173-7.
- Seo SH, Kim HJ, Oh SY, Lee JH, Suh KW. Computed tomography classification for parastomal hernia. Journal of the Korean Surgical Society. 2011;81(2):111-4.
- Hansson BM, Slater NJ, van der Velden AS, Groenewoud HM, Buyne OR, de Hingh IH, et al. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Annals of Surgery. 2012;255(4):685-95.
- Cingi A, Cakir T, Sever A, Aktan AO. Enterostomy site hernias: a clinical and computerized tomographic evaluation. Diseases of the colon and rectum. 2006;49(10):1559-63.
- Smietanski M, Szczepkowski M, Alexandre JA, Berger D, Bury K, Conze J, et al. European Hernia Society classification of parastomal hernias. Hernia : the journal of hernias and abdominal wall surgery. 2014;Feb, 18(1):1-6.
- Krogsgaard M, Pilsgaard B, Borglit TB, Bentzen J, Balleby L, Krarup PM. Symptom load and individual symptoms before and after repair of parastomal hernia: a prospective single centre study. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland. 2017;19(2):200-7.
- Krogsgaard M, Thomsen T, Vinther A, Gogenur I, Kaldan G, Danielsen AK. Living with a parastomal bulge - patients' experiences of symptoms. Journal of Clinical Nursing.
- Van Dijk SM, Timmermans L, Deerenberg EB, Lamme B, Kleinrensink GJ, Jeekel J, et al. Parastomal Hernia: Impact on Quality of Life? World journal of surgery. 2015.
- Kald A, Juul KN, Hjortsvang H, Sjödahl RI. Quality of life is impaired in patients with peristomal bulging of a sigmoid colostomy. Scandinavian Journal of Gastroenterology. 2008;43(5):627-33.
- Rubin MS, Bailey HR. Parastomal Hernias. In: Mackeigan JM, Cataldo PA, editors. Intestinal stomas Principles, techniques, and management. St. Louis, Missouri, United States of America.: Quality Medical Publishing, Inc; 1993. p. 245-67.
