Get full access with a free account
Benefits of the Coloplast® Professional Educational platform
![]() Full access to educational content, events and resources
Full access to educational content, events and resources
![]() Track your progress
Track your progress
![]() Share content with your colleagues
Share content with your colleagues
![]() Share supporting material with your patient
Share supporting material with your patient

How to assess 'the gap'
Knowing how to conduct an accurate wound assessment is absolutely key to wound healing.
Why it’s important to assess the gap
When you care for a patient with a chronic wound, your main goal is to help the wound to heal. Knowing how to conduct an accurate wound assessment is absolutely key here.
Inadequate wound assessments can lead to inappropriate treatment choices, poor patient outcomes and additional resource cost.1 Knowing what to look for when examining the wound – and the gap between the wound bed and the dressing – will give you a clearer sense of the condition of the wound and help you to decide how to create an optimal healing environment.
The Triangle of Wound Assessment is an important tool here. You can use it on all wound types, and it guides you in how to conduct a thorough assessment of the gap between the wound bed and the dressing. You can read more about the Triangle of Wound Assessment here.
How to assess the gap
You may have heard from your colleagues about the gap when assessing the wound. In this episode, you will learn about:
- What is the gap exactly?
- What are the risks associated with the gap?
- How do you assess the gap?
What to look for when assessing the gap
Before we look into the actual assessment process, it’s important to remember that effective wound management goes beyond the wound itself.
When caring for a patient with wounds – chronic or non-chronic – it always important to take a holistic approach. That means taking note of the patient’s overall medical history and health as well as the condition of the wound itself. If you need to refresh your knowledge of holistic wound management, visit the section here.
In a thorough assessment of the wound – and the gap between the wound and the dressing – you should consider:2
- how long has the patient had this wound?
- what is the wound’s aetiology (i.e. what caused it)?
- how is it healing? Do you see any signs of progress?
- what are the wound’s characteristics? Here you should look at:
- the wound’s depth, undermining, tunnelling and fistulas
- the underlying wound bed structure and topography
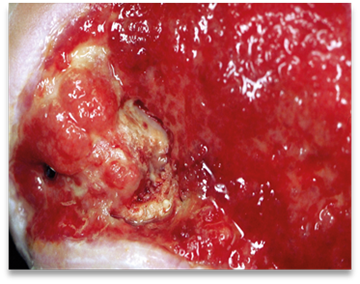
- the tissue quality. Are there signs of granulation or necrosis?
- the periwound (surrounding) skin and the wound edge
- the exudate, or fluid in the wound – its colour, consistency, odour and amount
If you notice that exudate is pooling, or if you believe that the exudate’s composition is preventing the wound from healing, your first priority should be to remove the excess exudate. Choosing the right wound dressing is the best way to do this. You can read more about how to do that here.
How often should I assess the gap?
You should complete a full assessment of a patient’s chronic wound at least once a week or, if possible, every time you change the dressing. This will help you diagnose and treat any wound infection in the early stages. By detecting an infection early on, you reduce the risk of serious complications, such as limb- or life-threatening infections.2
As you assess the wound, look for the following warning signs:
- exudate pooling, leakage and soiling 1, 3
- periwound skin damage (for example, maceration, skin stripping or erosion)
- delayed wound healing3
- signs of infection
- frequent dressing changes
Find out more about how to manage the gap here.
Exudate: The different types and colours
The following chart describes the different types of exudate. The wound’s exudate gives you important information about the wound’s health. If you notice an unexpected change in exudate characteristics, this may mean that there is a change in the wound’s status, e.g that the wound is infected. If this happens, you should re-evaluate the wound as quickly as possible.4, 3

Serous
Colour: Clear, amber or straw-coloured
Consistency: Thin, watery

Serosanguineous
Colour: Clear, pink to light red
Consistency: Thin, slightly thicker than water
Sanguineous
Colour: Red
Consistency: Thin, watery

Seropurulent
Colour: Cloudy, creamy, yellow, tan
Consistency: Thin

Fibrinous
Colour: cloudy
Consistency: Thin, watery

Purulent
Colour: opaque, milky, yellow, tan or brown, sometimes green
Consistency: Often thick

Haemopurulent
Colour: reddish milky, opaque
Consistency: Thick

Haemopurulent
Colour: Red, opaque
Consistency: Thick
